Intense Module 1
Introduction
EXPLANATORY NOTES
Advancement in Science and Technology, development of other systems of medicine and gaining world-wide recognition of Āyurveda needs us to think out of the box to develop new Instruments and Equipments for Pañcakarma following the golden rules laid in our classical texts. In Caraka Saṃhitā Sūtrasthāna Upakalpanīyam Adhyāya Caraka has described about Hospital building, treatment rooms, collection of various materials elaborately. He explains how and where a hospital building should be constructed.
REFERENCES IN UPAKALPANĪYAM ADHYĀYA
दृढं निवातं प्रवातैकदेशं सुखप्रविचारमनुपत्यकं धूमातपजलरजसामनभिगमनीयमनिष्ठानां च शब्दस्पर्शरसरूपगन्धानां सोदपानोदूखलमुसलवर्चःस्थानस्नानभूमिमहानसं वास्तुविद्याकुशलः प्रशस्तं गृहमेव तावत् पूर्वमुपकल्पयेत्||[i]
- Building should be strong and not exposed to winds
- Wind should be allowed to pass through only one passage.
- There should be comfortable moving space
- It should not be situated in a mountainous place nor should it be located near a bigger building.
- Building should not be exposed to smoke, sun, water, dust, noise.
- It shouldn’t have undesirable contacts, tastes, sight or smell.
- It should be well equipped with a water tank, mortar, pestle, latrine, bathroom and kitchen.
- An expert architect should design this building
There should be enough willing and skillful attendants for various purposes like cooking, bathing, massaging, lifting, seating of the patients and also for grinding of drugs. Caraka has also enumerated many birds, animals including cows to be kept here for serving various purposes.
There should be provision for
- Water vessel – Pātrī
- Spoon – Ācamanīya
- Water tub – Udakoṣṭha
- Big and Small earthen jars – Maṇika and Ghaṭa
- Frying Pan – Piṭhara
- Boiling Pan – Paryoga
- Small and Big Pitchers – Kumbhī – Kumbha
- Bowl – Kuṇḍa
- Saucers – Śarāva
- Ladles – Darvī
- Mat – Kaṭa
- Cover plate – Udañcana
- Cooking Pan – Paripācana
- Churning Stick – Manthāna
- Leather
- Cloth
- Thread
- Cotton
- Wool etc…
Arrangements should be done for beddings, seating etc. Bed sheet, Towel, Pillow and cushion should be kept there so as to facilitate lying flat, sitting, oleation, sudation, massage, unction, emesis, purgation, Asthāpana and Anuvāsana Basti, Nasya etc.
Other materials to be collected inside include Śastra, Dhūmanetra, Basti Netra, Uttarabasti Netra, scales and measuring instruments, Ghṛta, Taila, Vasā, Majjā, Mākṣika, Phāṇita, Saindhava, different kinds of Madya, milk preparations, Dhānyāmla, Ṣāṣṭika, Mudga, Māṣa, Yava, Tila, Kulattha, Badara, Mṛdvīkā, Kāśmarya, Parūṣaka, Triphala and other drugs employed in the Pañcakarma procedures.
………………नानाविधानि च स्नेहस्वेदोपकरणानि द्रव्याणि, तथैवोर्ध्वहरानुलोमिकोभयभाञ्जि, सङ्ग्रहणीयदीपनीयपाचनीयोपशमनीयवातहरादिसमाख्यातानि चौषधानि……[ii]
SNEHANA YANTRAS
There is detailed explanation regarding the Snehana Yantras, the Droṇī, Dhārā Pātra etc.. in Dhārā Kalpa.
TRADITIONAL DROṆĪ
Droṇī should be made of the heartwood of any of the below trees
प्लक्षोदुम्बरगन्धसारवरणन्य्ग्रोधदेवद्रुमा: पुन्नागाह्वकपित्थचोचबकुलाशोकासनाम्रस्तथा
दोलाचम्पकविल्वनिम्बखदिरामोघाग्निमन्थार्जुना:[iii]
- Plakṣa
- Udumbara
- Gandhasāra (Candana)
- Varaṇa
- Nyagrodha
- Devadruma
- Kapitha
- Aśoka
- Asana
- Āmra
- Bilva
- Nimba
- Khadira
- Amogha (Pāṭala)
- Agnimantha
- Arjuna
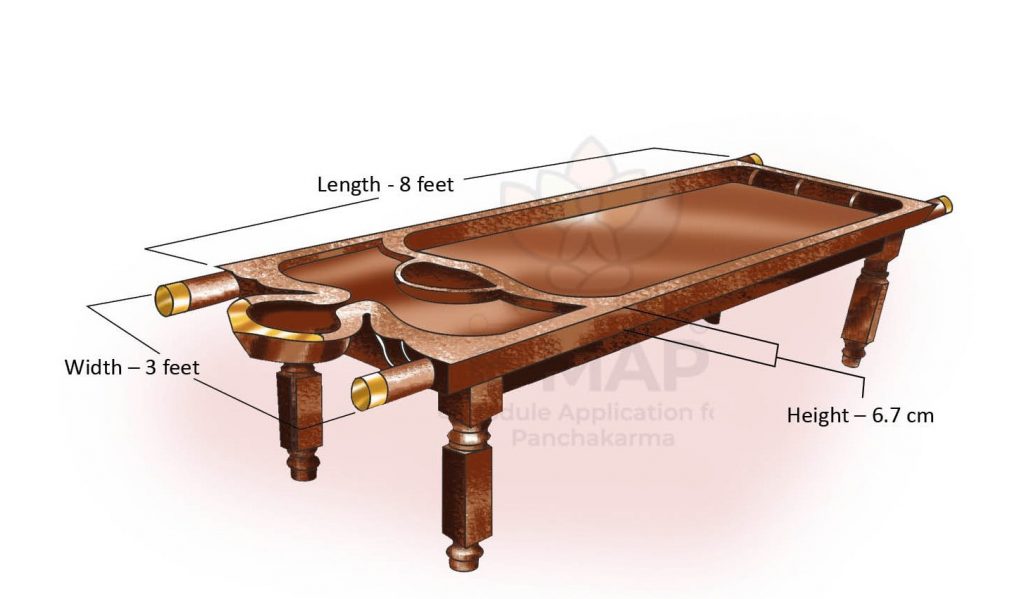
Measurements of Droṇī
Droṇī should be made by keeping surface area level.
द्रोणिहस्तचतुष्कदीर्घ करमात्रव्यास तत्पादमात्रोद्यत् भित्तियुतो ढृढा समतला पादान्तरन्थ्राबहि:[iv]
- 8 Hasta in Length (96 Aṅgula/72 inches / 6 feet)
- 1 Hasta width (18 inches)
- 6 Aṅgulas in height (4 and a half inches)
Droṇī should be having 2 compartments
- Proximal – Head end – Slightly elevated
- Distal – Foot End
- Should have an outlet at head and foot end to drain liquid out
- Length & Breadth of head part should be 18 inches.
- The limbs of Droṇī should be strong
Traditional Droṇī
[i] Cha.Su 15/6
[ii] Cha. Su 15/7
[iii] Dhārā Kalpa 3
[iv] Dhārā Kalpa 4
DHĀRĀ PĀTRA
The details regarding Dhārā Pātra is explained in Dhārā Kalpa as
स्वर्णाद्युत्त्मलोहजस्तु करको मृत्संभवो वा अत्र तत्
नालाग्रं तु कनिष्टकांगुलिपरिणाहोन्मितं रोगिण:
व्दिप्रस्थ: प्रमितो निधेय इति वा मध्यस्थरंध्रात् अधो
गच्चत् वर्तिरथोर्ध्वलंब्यपि घट: कार्य: शिर: सेचने [i]
- Made of material like gold, other superior metals or earthen ware
- Dhārā Pātra is wide mouthed, round bottomed vessel with a capacity of 2 Prastha
- Bottom of the vessel should have a perforation corresponding to the circumference of little finger of the patient
- The vessel should be suspended over the proximal end of Droṇī with cords tied around the rim of the vessel
- A wick of appropriate size should be suspended from the hole through which sneha dravya is falling as a Dhārā to the forehead of the patient.
धाराया: स्फ़टिकंसुवर्ण रजतप्लक्षादि पूर्वोक्त वृक्षायास्तु
ताम्रवराटिका प्रथितमृत्पात्रास्तु अतीवोत्तमा:
केचित् रोगि कनिष्टिकान्तविवरं शंसन्तिकेचित्तु वा
तत् पर्वोपमविस्तृतन्तु सुषिरं पात्रस्य मद्ध्येकृतम्
[i] Dhārā Kalpa 6
BASTI YANTRA
Basti Yantra comprises of Basti Netra and Basti Puṭaka
BASTI NETRA
It is made up of
- तयोस्तु नेत्रं हेमादिधातुदार्वस्थिवेणुजम्||
गोपुच्छाकारमच्छिद्रं श्लक्ष्णर्जु गुलिकामुखम्| [i] - सुवर्णरूप्यत्रपुताम्ररीतिकांस्यास्थिशस्त्रद्रुमवेणुदन्तैः |
नलैर्विषाणैर्मणिभिश्च तैस्तैर्नेत्राणि कार्याणि सु(त्रि)कर्णिकानि [ii]
For preparing Basti Netra having three Karṇikā (ridges) the following materials are used: gold, silver, copper, bronze, cow’s horn, bones of animals and others.
Characteristics of Basti Netra
- गोपुच्छाकारमच्छिद्रं श्लक्ष्णर्जु गुलिकामुखम्| [iii]
- ऋजूनि गोपुच्छसमाकृतीनि श्लक्ष्णानि च स्युर्गुडिकामुखानि
स्यात् कर्णिकैकाऽग्रचतुर्थभागे मूलाश्रिते बस्तिनिबन्धने द्वे| [iv]
The circumference of the nozzle at the base and top should be the same as that of the thumb and little finger of the patient of that age respectively. It should be straight and tapering like the tail of a cow. The mouth of the nozzle should be smooth and globular. One ring should be fixed at the level of one fourth from the top, and two other rings should be fixed at the base in order to facilitate tying the mouth of the bladder around the nozzle
[i] A. H. Su 19/9
[ii] Cha. Si 3/7
[iii] A. H. Su 19/9
[iv] Cha. Si 3/9
BASTI PUṬAKA
जारद्गवो माहिषहारिणौ वा स्याच्छौकरो बस्तिरजस्य वाऽपि|
दृढस्तनुर्नष्टसिरो विगन्धः कषायरक्तः सुमृदुः सुशुद्धः |
नृणां वयो वीक्ष्य यथानुरूपं नेत्रेषु योज्यस्तु सुबद्धसूत्रः[i]
The urinary bladder of the animals such as buffalo, sheep, goat, cow etc. should be used to prepare Basti (the holder bag of Basti Dravya).
Features: Dṛḍha (strong), Tanu (thin), Naṣṭa Sirā (devoid of veins), Vigandha (devoid of odour), Kaṣāyarakta (saffron-red), Sumṛdu (soft), Suśuddha a (well cleaned), and Yathanurūpa (size accordingly).
[i] Cha. Si 3/ 10
INTRODUCTION
NABH – National Accreditation Board for Hospitals and Health care providers
- It is a constituent board of Quality Council of India
- It is set up to establish and operate accreditation programme for healthcare organizations.
- NABH offers accreditation services to Hospitals, Small Health Care Organizations/Nursing Homes, Blood Banks, Wellness Centres and Medical Imaging Services.
- Accreditation of AYUSH Hospitals is a new initiative of NABH.
NEED FOR ACCREDITATION
- Concern for the quality of health care.
- Ayurveda Hospitals are an integral part of health care system and Accreditation would be the single most important approach for improving the quality of hospitals.
- Play expected roles in national health system.
BENEFITS OF ACCREDITATION
Benefits for Patients
- High quality of care and patient safety.
- Rights of patients are respected and protected.
- Patients satisfaction is regularly evaluated.
Benefits for Ayurveda Hospitals
- Stimulates continuous improvement.
- Enables hospital in demonstrating commitment to quality care.
- Raises community confidence in the services it provides.
- Provides opportunity to benchmark with the best.
Benefits for Hospital Staff
- Continuous learning
- Good working environment
- It improves overall professional development of staffs.
Benefits to Paying and Regulatory bodies
- Provides an objective system of empanelment by insurance and other third parties.
- Access to reliable and certified information on facilities, infrastructure and level of care.
NABH STANDARDS
Accreditation Standards | Structural Standards |
• It is based on three components- structure, process and outcome.
| • It basically deals with infrastructural requirements to help the organisations to deliver quality of care. |
• These standards measure the quality and safety aspects of the care delivered to the patients.
| • A minimum bed strength of 10 beds is essential for an Hospital to be considered for the Accreditation Program |
NABH STANDARDS for ayurveda hospitals
Patient centered standards
| Organization Centered Standards
|
1) Access, Assessment and Continuity of Care 2) Care of Patient 3) Management of Medication 4) Patient Right and Education 5) Hospital Infection Control
| 6) Continuous Quality Improvement 7) Responsibility of Management 8) Facility Management and Safety 9) Human Resource Management 10) Information Management System |
- Access, Assessment and Continuity of Care
- The Clinic defines and displays the services that it can provide.
- The Clinic has a defined patient registration process.
- Patients cared for by the organization undergo an established assessment before treatment
- Patient care is continuous and multidisciplinary in nature.
- Laboratory services, if provided, are monitored by the clinics.
- Care of Patient
- Care and treatment is provided in a uniform manner.
- Policies and procedures guide the Panchakarma Therapy
- The policies and procedures are documented.
- Documented policies and procedures exist to prevent adverse events like wrong site, wrong patient and wrong procedure.
- An informed consent is obtained by a consultant prior to the treatment process.
- Persons qualified are permitted to perform the procedures that they are entitled to perform.
- A brief note is documented prior to transfer of patient from Panchakarma Theatre.
- The consultant documents the post-procedure plan of care.
- A procedure to check the maintenance of Panchakarma Theatre.
- Guidelines for various Panchakrama therapies are prepared separately and adhered.
- Panchakarma therapies are done only in the presence of physician at the side.
- Patients with special needs & disabilities (vulnerable) shall be identified and treated accordingly
- Documented policies and procedures guide appropriate pain management.
- Documented policies and procedures guide appropriate rehabilitative services.
- Policies and procedures guide the care of patients undergoing parasurgical procedures like agnikarma, rakthamokshana, etc
- Policies and procedures guide all research activities.
- Patients are informed of their right to withdraw from the research at any stage and also of the consequences (if any) of such withdrawal.
- Patients are assured that their refusal to participate or withdrawal from participation will not compromise their access to the Clinic’s services
- Management of Medication
- Medication use is organized to meet patient needs and complies with applicable laws and regulations.
- Medication prescription, dispensing and administration follow standardized processes to ensure patient safety.
- Noncompliance to drugs and adverse effects & the medication errors, if any, are appropriately addressed.
- Patient Right and Education
- The Clinic protects patient and family rights.
- A documented process for obtaining patient and / or families consent exists for informed decision making about their care.
- Patient and families have a right to information and education about their healthcare needs.
- They also have a right to information on expected costs.
- Hospital Infection Control
- Infection control practices and adherence to standard precautions and hygienic practices shall be observed at all times in the clinic.
- The Clinic complies with Bio Medical Waste Management Rules and associated regulations.
- Bio Medical waste is collected, handled, segregated and disposed of as per the
- Staff is trained to handle BMW and follow precautions.
- Continuous Quality Improvement
- There is a structured quality improvement and continuous monitoring programme.
- The clinic identifies key indicators which are used as tools for continual improvement.
- Responsibility of Management
- The hospital shall identify a responsible person, who has the defined responsibility and authority to ensure that the quality programme is maintained.
- The hospital is managed by the leaders in an ethical manner.
- The hospital initiates and maintains a patient record for every patient.
- Those responsible for management should have addressed all applicable aspects of human resource management.
- Facility Management and Safety
- The Clinic’s environment and facilities operate to ensure safety of patients, their families and staff.
- The Clinic has a programme for equipment management, safe water, electricity, medical gases and vacuum system as applicable.
- The Clinic has plans for emergencies (fire and non-fire) and hazardous materials within the facilities.
- Human Resource Management
- Should address all applicable aspects of human resourse management.
- Information Management System
- The clinic should have a well occupied information management system
STRUCTURAL GUIDELINES FOR PANCHAKARMA HOSPITAL
- SPACE REQUIREMENT
- Reception and waiting area (500 sq ft) – 1
- Consultation room (100 sq ft) – 1
- Pharmacy (300 sq ft) – 1
- Panchakarma therapy room (100 sq ft) – 2
- (male and female)
- Post therapy room (100 sq ft) – 2
- (male and female)
- Store/kitchen (250 sq ft) – 1
- IP wards and rooms – Min 10 beds
- Man power requirements
- Ayurvedic doctor – 1
- Trained technician for ayurvedic panchakarm – 3 + 3
- Receptionist to perform registration and enquiries- 1
- Pharmacist – 1
- Housekeeping staff for cleaning- 1
- Attender – 1
- EQUIPMENTS & FURNITURE
· Massage table: 7×3 feet · Droni with stand: wooden or fibre 9×3 feet · Steam cabin with steam generator · Gas stove · Shirodara pot with stand · Shiravasti cap · Pressure cooker · Leech tank · Leeches for leech therapy · Instrument for agni karma · Vasti yantra · Disposable enema 200ml and 600ml capacity required as per daily use · Uttaravasti yantra
| · Emesis can · Chair · Refrigerator · Linen towels, bed sheets, blankets, thin clothes for various therapeutical preparations like kizhi etc. · Aprons, disposable under garments, disposable gloves required as per use. · Necessary vessels for various medical preparations · Stainless steel utensils of 2, 5, 8, 10 litre capacities · Spoons, jugs, storage vessels etc. as required. · Computer with printer
|
NABH ACCREDITED AYUSH HOSPITALS
- AyurVaid Hospital, Domlur Extension, Bangalore, Karnataka
- Maharishi Ayurveda Hospital, Khosla Medical Institute & Research Society, New Delhi
- Amala Ayurvedic Hospital & Research Centre, Thrissur, Kerala
- Sreedhareeyam Ayurvedic Eye Hospital & Research Centre, Ernakulam, Kerala (Renewal Under Process)
- Soukya Indian Holistic Health Centre Pvt. Ltd., Bangalore, Karnataka
- AyurVaid Hospital, Ramamurthy Nagar Extn., Bangalore, Karnataka
- Sahaya Holistic Integrative Hospital Pvt. Ltd., Bangalore, Karnataka
- Punarnava Ayurveda Hospital Pvt. Ltd., Edappally North, Cochin, Kerala
- Kalari Kovilakom, Kollengode, Palakkad, Kerala
- I-AIM Healthcare centre ( IHC), Bangalore, Karnataka
- Ashtavaidyan Thaikkattu Mooss Vaidyaratnam Nursing Home, Thrissur, Kerala
- Nagarjuna Ayurvedic Centre Ltd., Ernakulam, Kerala
DEFINITION
According to Biomedical Waste (Management and Handling) Rules, 1998 of India “Any waste which is generated during the diagnosis, treatment or immunization of human beings or animals or in research activities pertaining thereto or in the production or testing of biologicals.
Biomedical wastes can be in both solid and liquid forms. Examples of biomedical wastes include:
- Waste sharps such as needles, lancets, syringes, scalpels, and broken glass
- Human tissues or identifiable body parts (as a result of amputation)
- Animal tissues and waste from veterinary hospitals
- Used bandage, dressings, gloves, and other medical supplies
- Liquid waste from infected areas
- Laboratory wastes
Biomedical wastes are distinct from regular garbage and require particular disposal and treatment.
TYPES OF BIOMEDICAL WASTE
The World Health Organization (WHO) has categorized biomedical waste into eight categories. They are:
- Infectious Waste – Any biomedical waste that is infectious or contaminated.
- Sharps – Sharps objects like needles, scalpels, broken glass, and razors.
- Pathological Waste – Body parts of humans or animals, including tissues, fluids, or blood.
- Pharmaceutical Waste – Unused drugs, medicine, or creams that are expiring.
- Genotoxic Waste – Toxic drugs and hazardous toxic waste
- Radioactive Waste – Any waste containing potentially radioactive materials
- Chemical Waste – Liquid waste from machines, batteries, and disinfectants is chemical.
- General/Other Waste – All other non-hazardous waste.
Further, the Central Pollution Control Board (CPBC) has designated separate colour-coded bins to dispose of biomedical wastes as per their nature.
- Yellow Bin: For anatomical waste, chemical waste, soiled waste, chemotherapy waste, discarded linen and medicines, and laboratory waste.
- Red Bin: For contaminated plastic wastes
- Blue Bin: For glass waste and metallic implants
- Black Bin: For hazardous and other waste
The wastes in each of the bins have different treatment and disposal methods.
EFFECTS OF BIOMEDICAL WASTE
Exposure to hazardous biomedical waste can cause disease or injury to human health. HIV, hepatitis B, and C are the three most commonly spread viruses worldwide due to improper treatment of medical wastes. They are transmitted through injuries from contaminated syringes and needles.
Doctors, nurses, and sanitation workers are amongst the most vulnerable to the harmful effects of biomedical waste.
BIOMEDICAL WASTE MANAGEMENT PROCESS
The hospital waste like body parts, organs, tissues, blood and body fluids along with soiled linen, cotton, bandage and plaster casts from infected and contaminated areas are very essential to be properly collected, segregated, stored, transported, treated and disposed of in safe manner to prevent nosocomial or hospital acquired infection.
- Waste collection
- Segregation
- Transportation and storage
- Treatment & Disposal
- Transport to final disposal site
- Final disposal
BIOMEDICAL WASTE TREATMENT AND DISPOSAL
- Incineration Technology
- Non-Incineration Technology
- Autoclaving
- Microwave Irradiation
- Chemical Methods
- Plasma Pyrolysis
INCINERATION TECHNOLOGY
This is a high temperature thermal process employing combustion of the waste under controlled condition for converting them into inert material and gases. Incinerators can be oil fired or electrically powered or a combination thereof. Broadly, three types of incinerators are used for hospital waste: multiple hearth type, rotary kiln and controlled air types. All the types can have primary and secondary combustion chambers to ensure optimal combustion. These are refractory lined.
NON-INCINERATION TECHNOLOGY
Non-incineration treatment includes four basic processes: thermal, chemical, irradiative, and biological. The majority of non-incineration technologies employ the thermal and chemical processes. The main purpose of the treatment technology is to decontaminate waste by destroying pathogens. Facilities should make certain that the technology could meet state criteria for disinfection.
AUTOCLAVING
- The autoclave operates on the principle of the standard pressure cooker.
- The process involves using steam at high temperatures.
- The steam generated at high temperature penetrates waste material and kills all the micro organism
- These are also of three types: Gravity type, Pre-vacuum type and Retort type.
In the first type (Gravity type), air is evacuated with the help of gravity alone. The system operates with temperature of 121 deg. C. and steam pressure of15 psi. for 60-90 minutes. Vacuum pumps are used to evacuate air from the Pre vacuum autoclave system so that the time cycle is reduced to 30-60 minutes. It operates at about 132 deg. C. Retort type autoclaves are designed much higher steam temperature and pressure. Autoclave treatment has been recommended for microbiology and biotechnology waste, waste sharps, soiled and solid wastes. This technology renders certain categories (mentioned in the rules) of bio-medical waste innocuous and unrecognizable so that the treated residue can be land filled.
MICROWAVE IRRADIATION
- The microwave is based on the principle of generation of high frequency waves.
- These waves cause the particles within the waste material to vibrate, generating heat.
- This heat generated from within kills all pathogens.
CHEMICAL METHODS
- ́1 % hypochlorite solution can be used for chemical disinfection
PLASMA PYROLYSIS
- Plasma pyrolysis is a state-of-the-art technology for safe disposal of medical waste. It is an environment- friendly technology, which converts organic waste into commercially useful byproducts. The intense heat generated by the plasma enables it to dispose all types of waste including municipal solid waste, biomedical waste and hazardous waste in a safe and reliable manner. Medical waste is pyrolysed into CO, H2, and hydrocarbons when it comes in contact with the plasma-arc. These gases are burned and produce a high temperature (around 1200oC).